The "Anxiety" Misdiagnosis: A Case of Mistaken Identity
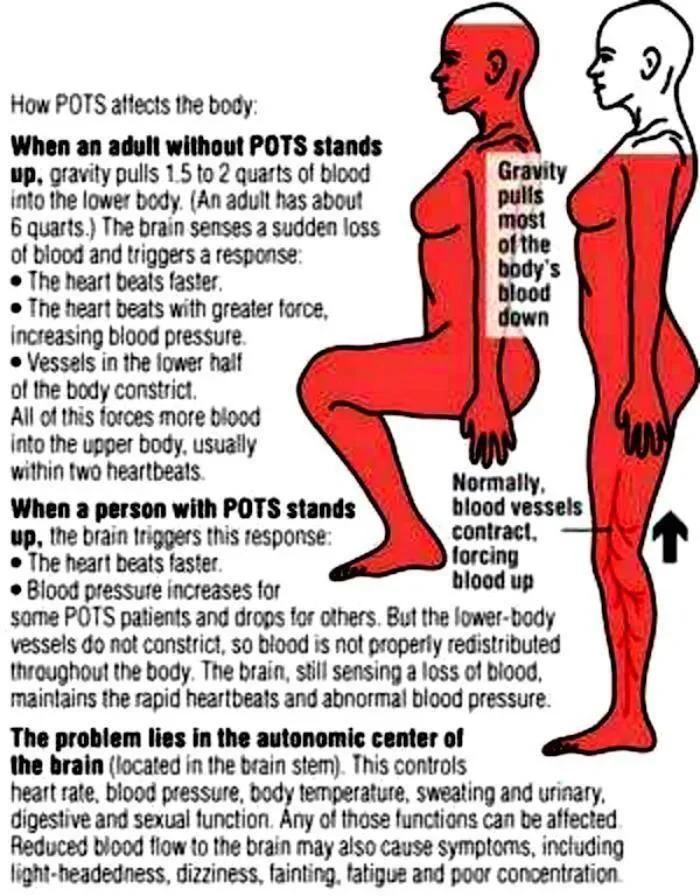
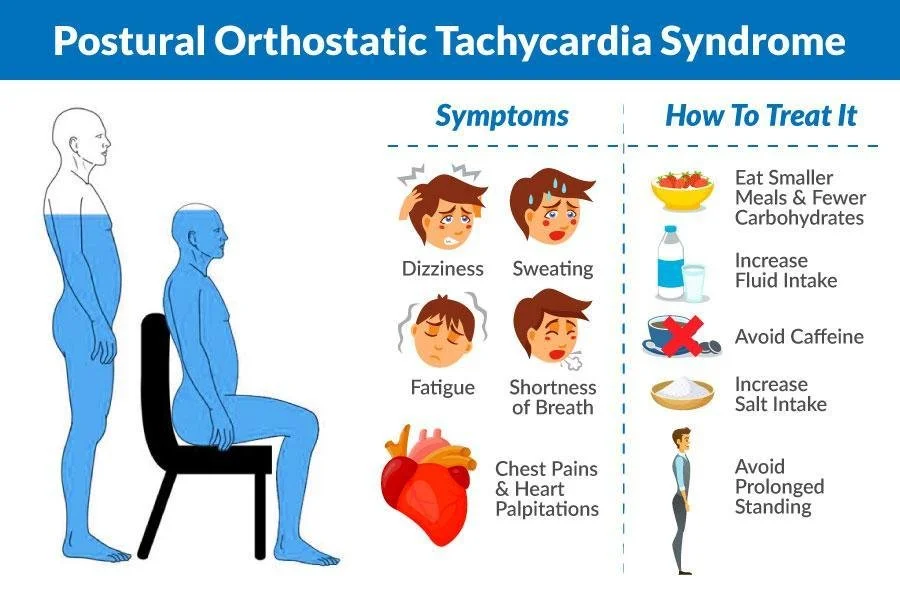
Because POTS causes a racing heart, shortness of breath, and sweating, it mimics the physical symptoms of anxiety and panic attacks. Millions of POTS patients—especially women—are told they have Anxiety, Panic Disorder, or ADHD. They are prescribed SSRIs or therapy for "stress," while their actual physiology is being ignored.
Here is the difference:
Anxiety: Starts in the mind (fear) and triggers the body.
POTS: Starts in the body (standing up) and triggers the mind.
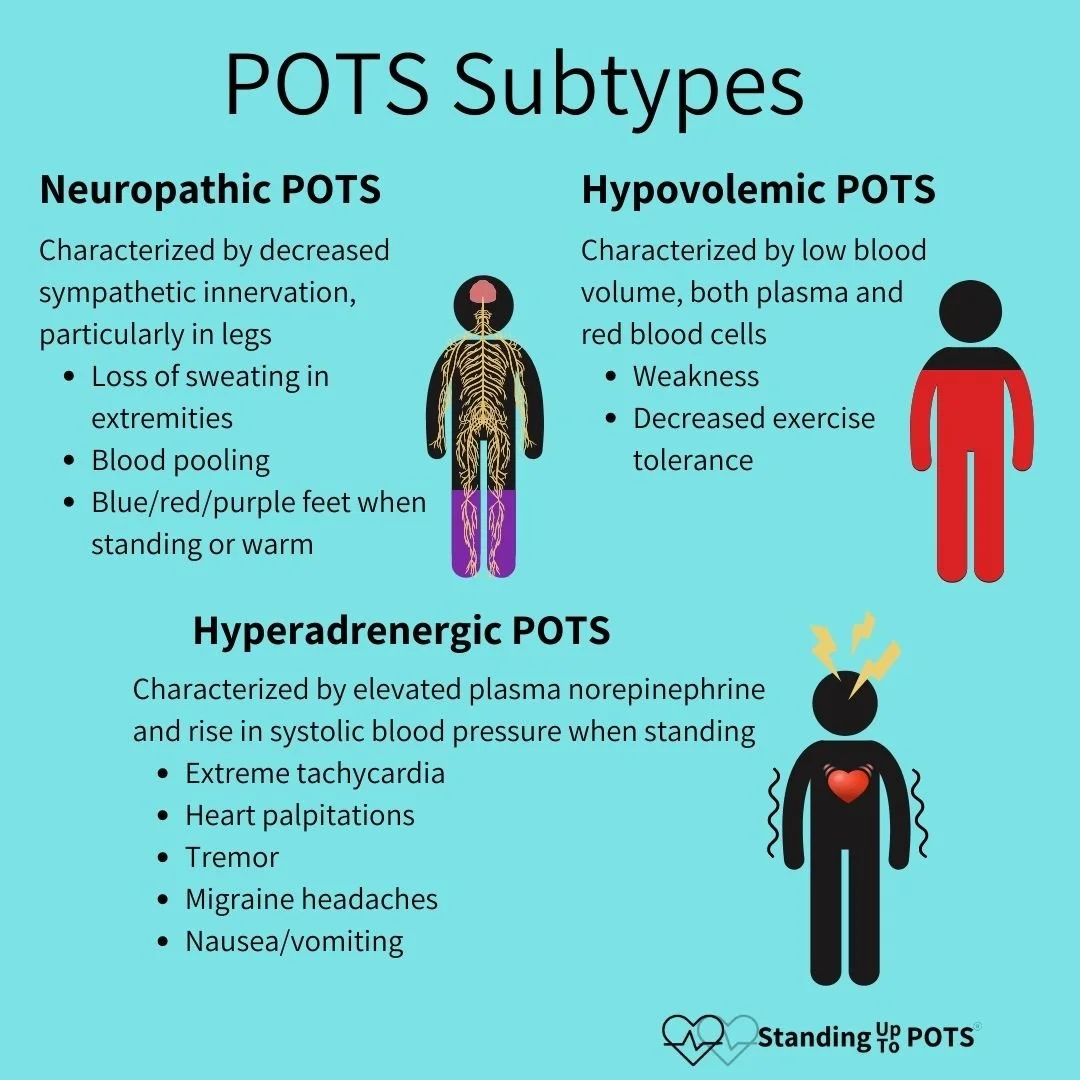
I specialize in Hyperadrenergic POTS (Hyper-POTS). This is a specific subtype where the body dumps massive amounts of Norepinephrine (adrenaline) upon standing. This creates a chemical sensation of Terror or Rage that has nothing to do with your emotions. It is a biological event. I help you untangle the "Chemical Anxiety" from true emotional anxiety so you can stop gaslighting yourself.
The "Trifecta" Link
POTS rarely travels alone. If you have POTS, we will also screen for:
Ehlers-Danlos Syndrome (EDS): Stretchy veins lead to blood pooling.
MCAS: Histamine dumps can trigger tachycardia.
ME/CFS: The energy crash that follows the adrenaline spike.
I view POTS through the lens of the RCCX Theory—understanding that your high-voltage nervous system is prone to these autonomic glitches.
My Approach: Pacing & Nervous System Regulation
While Cardiologists treat the heart rate and blood pressure issues (Beta-blockers, Salt, Fluid), I treat the Life Impact
1. The Psychology of Pacing Pacing isn't just "resting." It is a rigorous discipline of energy management. We work together to map your "Energy Envelope." We identify the cognitive, physical, and emotional costs of your day, and we restructure your life to prevent the "Push-Crash" cycle.
2. Somatic Regulation We use tools to manually down-shift your nervous system from Sympathetic (Fight/Flight) to Parasympathetic (Rest/Digest).
Compression therapy
Vagus Nerve Stimulation and Vagal Toning Exercises
Breathwork for Dysautonomia: Learn how to use your own breath to switch from fight/flight into rest/digest.
Horizontal Therapy: Learning to live a full life while embracing that sometimes that means being horizontal a lot (Think accommodations such as lay down desk/workstation or chair where you can sit “criss cross applesauce” or a counterstool next to the stove so you can sit while chopping/cooking.
3. Grieving the "Vertical" Life POTS is an identity crisis. You may have been an athlete, a dancer, or a busy professional. We process the grief of losing your physical freedom, and we work to build a new identity that honors your current capacity without defining you by your limitations.
4. Baseline improvement: With appropriate medical and and lifestyle interventions, POTS symptoms can be well managed and it is even possible to increase your baseline over time. There is hope!
You are not lazy. You are not crazy. You are fighting gravity. And I am here to help you win.